~ Drs. Saira, Anil Cherian, Ezer Kang, Darcie A.P. Delzell, Paul E. McNamara, and Joel Cuffey
ABSTRACT:
Poor mental health functioning among persons living with HIV (PLHIV) has gained considerable attention particularly in low-income countries that disproportionately carry the global HIV/AIDS burden. Fewer studies, however, have examined the relationship between poverty indicators and mental health among PHLIV in India. Based on this cross-sectional study of 196 HIV-seropositive adults who received medical services at Shalom AIDS Project in Delhi, India, structural equation modeling and mediation analysis were employed to estimate the associations between poverty indices (household asset index, food security, unemployment, water treatment, sanitation), HIV-health factors (illness in the past 3 months, co-morbid medical conditions), and psychological distress. In the final model, ownership of fewer household assets was associated with higher levels of food insecurity, which in turn was associated with higher psychological distress. Also, the household asset index, food insecurity, and unemployment had a larger effect on psychological distress than new opportunistic infections. These findings build on increasing evidence that support concerted efforts to design, evaluate, and refine HIV mental health interventions that are mainstreamed with livelihood programming in high poverty regions in India.
Introduction
Poor mental health functioning among persons living with HIV (PLHIV) has gained considerable attention particularly in low-income countries that disproportionately carry the global HIV/AIDS burden. India has the third largest number of PLHIV in the world – 2.1 million (1.7–2.7 million) at the end of 2013, which accounts for approximately 4 out of 10 people living with HIV in the region (UNAIDS, 2014). Although the numbers of new HIV infection have declined by 19%, India accounted for 38% of all new HIV infection in South and Southeast Asia regions and 51% of AIDS-related deaths (UNAIDS, 2014).
Recent cross-sectional studies examining psychological distress among PLHIV in India have indicated rates of 5% (n = 1934 in Goa; Mayston et al., 2014) to 79% (n = 227 in Udipi; Kamath, Robin, & Chandrasekaran, 2014) depending on the sampling and on how mental health was measured. Predictors of poor mental health functioning among PLHIV in India have been associated with family (conflictual relationships, spousal AIDS diagnosis) and individual factors (physical illness symptoms – pain, concurrent alcohol abuse; Chandra, Ravi, Desai, & Subbakrishna, 1998), low self-esteem (Jagannath et al., 2011), divorced, separated, or widowed marital status, and socio-cultural related stressors (internalized, experienced, and perceived HIV stigma; Zelaya et al., 2012).
Fewer studies, however, have examined the potential relationship between poverty indicators and mental health among PHLIV in India. This relationship is important to consider given that in 2010 one-third of the world's 1.2 billion extreme poor (defined by the World Bank as living on less than $1.25 a day) resided in India (UN, 2014). Moreover, individuals living in concentrated poverty who experienced adverse events or “shocks” such as poor physical health or widowhood were at significantly higher risk of mental health problems compared to those who had not (Das, Do, Friedman, McKenzie, & Scott, 2007). This highlights the importance of examining what and how specific poverty indicators potentially heighten the vulnerability to poor mental health among PLHIV (Lund et al., 2010).
Numerous explanatory models that accounted for the poverty–mental health relationship suggested that indicators such as unemployment, low education, having no electricity or tap water, or overcrowded living environment predicted poor mental health outcomes in the majority world (Patel & Kleinman, 2003). Recent studies have also argued for a methodological shift from income-based to asset-based measurements of poverty and well-being, particularly in countries where household income and expenditures are less accurate estimates of economic well-being (Sahn & Stifel, 2003). Based on the National Family Health Survey (NFHS), for example, that sampled 88,000 households in India on 21 asset indicators categorized into consumer durables (e.g., radio, television), household residence characteristics (e.g., building material, source of drinking water), and household ownership, findings indicated that on average children from households with a higher asset index score were 31 percentage points more likely to enroll in school than children from lower asset household scores (Filmer & Pritchett, 2001).
Another measure of poverty that has gained increased attention in HIV outcome studies is food security. Various studies have converged on the definition of household food security as the access through socially/culturally acceptable means at all times to sufficient food to meet basic dietary needs required for an active and healthy and productive life (Anderson, 1990). It has been well established that compared to the general population, food insecurity estimates among PLHIV living in low- and high-resource regions were notably higher (Anema, Vogenthaler, Frongillo, Kadiyala, & Weiser, 2009). This is potentially accounted for by decreased household labor when a productive family member's HIV illness debilitates their physical capacity to maintain gainful employment, often resulting in the purchase of poorer quality of food (Bukusuba, Kikafunda, & Whitehead, 2007). However, in the context of HIV-affected communities, food security cannot be treated independent of broader competing daily necessities such as transportation or child education costs, particularly for women (Maxwell & Smith, 1992). The cumulative “uncertainty in the household ecology” (Weaver & Hadley, 2009; p. 266) coupled with the amplified othering and marginalization of households with less food security have been found to be associated with poorer mental health functioning (Subbaraman et al., 2014). Cross-sectional studies have also highlighted an association between food insecurity and depression among PLHIV living in resource limited African countries (Hadley et al., 2008; Tsai et al., 2012). The only study of PLHIV in India found an association between household food insecurity and lower quality of life and more depressive symptoms specifically among men (Heylen, Panicker, Chandy, Steward, & Ekstrand, 2014).
Given the dearth of studies examining the relationship between multiple poverty indices and mental health functioning among adults living with HIV in India, this cross-sectional study will investigate the association between poverty measures and psychological distress outcomes among a convenience sample of adults receiving HIV-medical and supportive services at a community HIV clinic in Delhi, India. Specifically, it is hypothesized that psychological distress will be associated with poverty indices (household economic status [asset index], food security, unemployment, water treatment, sanitation) to a greater degree than factors related to health (illness in the past 3 months, co-morbid medical conditions).
Methods
Participants
Adults over 18-years of age with a confirmed HIV-seropositive diagnosis receiving outpatient medical and/or home-based supportive services at Shalom Delhi, a community faith-based in- and outpatient HIV clinic in Delhi, were eligible to participate in this study. Patients are generally referred to Shalom Delhi by government hospitals for maintenance of HIV opportunistic infections and general medical care. Patients with acute illness are admitted for inpatient treatment until they regain their strength to return home. Between April 2007 and March 2008, 222 consented and completed the individual interviews at the clinic during a scheduled visit.
Procedure
Two Institutional Review Boards at each of the participating sites approved the research protocols. Site medical providers identified potential participants by reviewing patient charts and medical appointment schedules for eligibility requirements. Validated instruments were translated from English to Hindi by a translator and back translated to English by a second independent translator. The medical site staff was trained to explain the informed consent protocol and administered the face-to-face individual interviews during participant's routine medical appointments or scheduled study visit at the clinic.
Measures
Dependent variable
Psychological distress. The K6 screening scale of non-specific psychological distress, a validated brief screener for the presence of serious mental illness in the general population, was the primary outcome measure (Kessler et al., 2003). K6 validation studies were conducted in India where administration of a longer psychiatric assessment was not feasible, and found to be a valid diagnostic measure of psychological distress (Kessler et al., 2010). The K6 consists of six questions that rate the frequencies of experiencing nervousness, hopelessness, restlessness, depression, required effort in completing activities, and worthlessness in the past 30 days. Participants responded on a 5-point Likert scale ranging from 0 (none) to 4 (all the time). Raw scores ranged from 0 to 24 with higher scores indicating more severe symptomatology.
Independent variables
Household asset. Household asset was an index constructed from a principal components factor analysis (PCA) of responses to the question “does your household own any of these [17] items” including appliances (e.g., washing machine, refrigerator, air conditioner, and mobile phone) and other household resources (e.g., motorcycle, bicycle). Filmer and Pritchett (2001) constructed this asset index and proposed using PCA to determine the weights for each index variable based on the NHFS conducted in India, which sampled approximately 88,000 households. The first component obtained from our analysis accounted for 23% of the variance in household asset ownership. Asset weights for each household item were calculated with higher index values representing higher levels of relative wealth (see Table 1).
Table 1. Asset index weights.
| Asset | Weight |
|---|---|
| Color television | 0.724 |
| Radio/cassette/CD player | 0.637 |
| Camera/camcorder | 0.341 |
| Pressure lamp (Lantern) | –0.403 |
| Telephone/mobile phone | 0.640 |
| Bicycle | 0.015 |
| Motorcycle/scooter | 0.467 |
| Sewing machine | 0.359 |
| Motorcar, etc. | 0.413 |
| Pressure cooker | 0.280 |
| Refrigerator or freezer | 0.682 |
| Watches | 0.447 |
| Washing machine | 0.412 |
| Air conditioning | 0.375 |
| Fan | 0.342 |
| Heater/cooler | 0.715 |
| Black-and-white television | –0.247 |
Food insecurity. The Household Food Insecurity Access Scale (HFIAS; Coates, Swindale, & Blinsky, 2007) consisted of nine occurrence questions (e.g., Did you worry that your household would not have enough food [in the past 30 days]?) and nine frequency of occurrence follow-up questions that were asked to determine how often the condition occurred in the past 30 days on a 3-point Likert scale (1 = rarely and 3 = often). The HFIAS occurrence questions assessed three domains of food insecurity – anxiety/uncertainty about the household food supply, insufficient quality of food, and insufficient food intake and its physical consequences. A total HFIAS continuous score was calculated by summing the codes for each frequency-of-occurrence item. The maximum score for a household was 27 and the minimum score is 0. The higher the score, the more food insecurity the household experienced.
Health information. The following participant health information was obtained by interviews and medical chart review: current antiretroviral medication treatment (yes/no), opportunistic infections in the past 6 months, occurrence and frequency of HIV illness symptoms in the past 3 months, and diagnosis of non-HIV illness.
Socio-demographic household characteristics. Participants provided the following information during the interview: age, sex, marital status, household size, number of household dependents, employment status, and education. Living standard levels were measured by assessing the availability and location of plumbing, and drinking water access and source.
Data analysis
Twenty-six cases were excluded from the current analyses due to missing data for food security, mental health, or household asset index scores, resulting in a sample of 196. An initial set of 17 potentially influential independent variables was identified via graphical assessment. A full multiple regression model was performed with these variables in the R programming environment (R Core Team, 2014). An extra-sum-of-squares test was performed to compare the full regression model with a reduced model that included only the statistically significant factors that meaningfully explained the variability in psychological distress scores. As an additional check, a stepwise regression procedure was performed with the general Akaike Information Criterion and the final model including the same independent variables as the one resulting from the extra-sum-of-squares tests. Structural equation modeling (SEM) techniques were then employed using Mplus (Muthén & Muthén, 2012) to also model the mediation portion of the analysis. The Comparative Fit Index (CFI), the root mean squared error of approximations (RMSEA), and a chi-square fit statistic were calculated to assess the overall model fit. The CFI specifically indicated the practical fit of the model to the data with a good fit value of 0.95 or higher. Values of RMSEA of <0.08 implied an acceptable model fit and values of <0.05 implied a good fit (Browne & Cudeck, 1990). In the present study, 90% confidence intervals for the RMSEA measures are presented. Small values of the chi-squared test statistic, along with the small associated p-value indicate good model fit.
Results
Participant characteristics
Two hundred twenty-two adults living with HIV consented to participate in this study. Twenty-six cases were removed from the analysis due to missing data for asset index, food security, and psychological distress measures. The final analysis was performed with 196 complete cases (see Table 2 for participant characteristics).
Table 2. Descriptive statistics of study variables, n = 196.
| Characteristics | % (n) | M (IQR) |
|---|---|---|
| Gender | ||
| Male | 54% (106) | |
| Female | 45% (88) | |
| Single parent (yes) | 27% (53) | |
| Age | 34 (28–38) | |
| Years of education | 9 (3–13) | |
| Number of children in household | 2 (1–3) | |
| Unemployed in past 12 months | 4% (8) | |
| Plumbing in house (yes) | 73% (144) | |
| Latrine in house (yes) | 69% (135) | |
| Public trash collection (yes) | 64% (145) | |
| Opportunistic infection in past 6 months | 61% (119) | |
| Other non-HIV illness | 47% (92) | |
| Current ARV treatment (yes) | 44% (86) | |
| Number of times sick in past 3 months | 2 (1–2) | |
| Psychological distress in past 30 days (K6) | 12 (11–14) | |
| Food security (HFIAS) | 9 (8–11) | |
| Household Asset Index | 0 (-2 to 1) | |
Model selection with multiple regressions
The results of the full multiple regression analysis are found in Table 3. A reduced model only including the statistically significant variables was compared with the full model using an extra-sum-of-squares test. The resulting p-value of 0.97 indicated that the reduced model contained all of the influential independent variables. Variables shown to influence psychological distress were household asset index, food insecurity, unemployment, and new opportunistic infections in the past 6 months. Specifically, lower psychological distress was independently associated with lower household asset index, higher food insecurity, being unemployed, and receiving a diagnosis of new opportunistic infection in the past 6 months.
Table 3. Full regression model predicting psychological distress.
| Independent variable | Estimate | p-value |
|---|---|---|
| Gender | 0.51 | 0.61 |
| Age | –0.01 | 0.77 |
| Education | 0.02 | 0.81 |
| Unemployment (yes/no) | 2.96 | 0.02 |
| Number of dependents (logged) | –0.21 | 0.50 |
| Household size (logged) | –0.10 | 0.87 |
| New opportunistic infection (yes/no; past 6 months) | –1.48 | 0.02 |
| Occurrence of illness (past 3 months) | 0.25 | 0.69 |
| Frequency of illness (past 3 months) | 0.15 | 0.56 |
| Current antiretroviral treatment | –0.23 | 0.63 |
| Other non HIV-related illness | –0.13 | 0.80 |
| Watersource | 0.65 | 0.20 |
| Sanitation | –0.47 | 0.38 |
| Food insecurity | 0.35 | <0.001 |
| Household Asset Index | –0.38 | 0.01 |
| Gender and education interaction | –0.05 | 0.62 |
SEM and mediation analysis
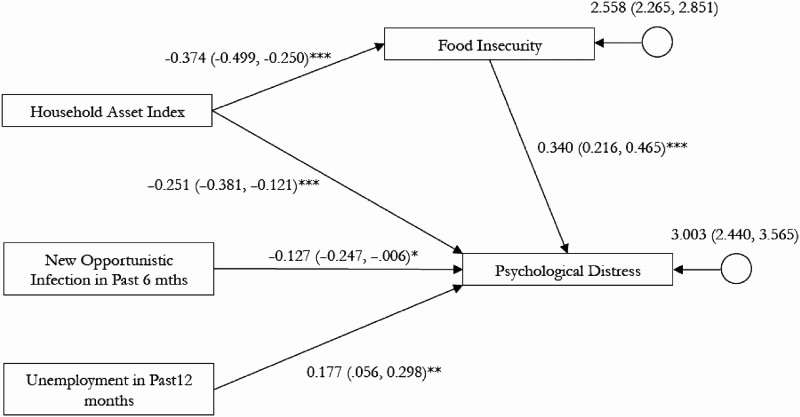
To investigate the direct and indirect associations between psychological distress, poverty measures, and illness factors, we simultaneously estimated coefficients for all the variables together as shown in Figure 1. The results indicated a good model fit, χ2 = 1.78 (p-value = 0.41); CFI = 1.00, 90% RMSEA confidence interval = 0.00, 0.14. As evidenced by the larger standardized coefficients (see Figure 1), household asset index, food insecurity, and unemployment have a larger effect on psychological distress than new opportunistic infections. Also, lower household asset index was both directly and indirectly associated with higher psychological distress through higher level of food insecurity. The results of the model fit are shown in Figure 1.
Figure 1. Structural equation model showing direct and indirect effects on psychological distress. Note: standard coefficients are depicted, *p < .05. **p < .01. ***p < .001.
Discussion
The relationship between mental health and poverty among PLHIV in both high- and low-income countries has drawn timely implications for integrative programming particularly in regions with high rates of poverty and HIV prevalence (Heylen et al., 2014). Our finding of a significant relationship between increased household asset-ownership and decreased psychological distress is consistent with previous studies (Heylen et al., 2014; Myer, Stein, Grimsrud, Seedat, & Williams, 2008; Patel, Kirkwood, Pednekar, Weiss, & Mabey, 2006). This study adds to these previous findings by demonstrating that among PLHIV, household asset-ownership, unemployment, and food insecurity were more strongly associated with psychological distress than onset of opportunistic infections in the past 6 months. Particularly for PLHIV who contend with competing stressors of poverty and HIV illness management, the immediacy of needs related to food security and other daily livelihood concerns often overshadow the chronicity of HIV-health concerns.
Our analysis also indicated that poverty as measured by ownership of fewer household assets was associated with higher levels of food insecurity, which in turn was associated with higher psychological distress. This finding aligns well with the structural vulnerability framework that proposes an association between poverty and mental health outcomes through pathways such as stressful life circumstances, deprivations, or “shocks” (Patel & Kleinman, 2003) from which persons have limited capacity to recover (Baro & Deubel, 2006). It is arguable that in poor households affected by HIV, food insecurity poses as such a stressor, particularly when it has been compromised by sudden adverse events (Das et al., 2007), such as physical debilitation of productive household members and increased caregiver burden due to HIV illness (Anema et al., 2009; Baro & Deubel, 2006; Bukusuba et al., 2007). Moreover, the additive effect of HIV-related stressors on well-established consequences of food security such as alienation and social deprivation, minimized agency, guilt and shame for not being able to provide for one's family conceivably heighten anxiety and depressive markers (Hadley & Patil, 2006; Nanama & Frongillo, 2012). Our findings provide modest support for integrative mental health programming that co-address alleviation of psychological distress symptoms and promotion of sustainable livelihood strategies that reduce food insecurity (e.g., employment creation) – one that does not minimize either the importance of individual-level mental health intervention or broader poverty alleviation programs in India. The indirect benefits of socio-economic empowerment initiatives such as microfinance and vocational training in the Asia-Pacific region on improved quality of life and increased self-esteem of PLHIV are well established (United Nations Development Programme, 2012). Moreover, there is growing evidence that support inter-sectoral models that integrate mental health services in primary care settings in low- and middle-income countries (World Health Organization, 2003). However, there has been less programmatic urgency to “piggyback” or mainstream mental health care onto existing livelihood initiatives (Patel, 2007, p. 93). Our findings further strengthen the rationale to innovatively address the link between socio-economic livelihood and mental health and to critically consider programmatic lessons gleaned from the growing number of integrated programs in African countries (Aberman, Rawat, Drimie, Claros, & Kadiyala, 2014).
The unexpected relationship between increased onset of opportunistic infections and lowered psychological distress is suggestive of how PHLIV receive perhaps a wider range of supportive services during an illness episode. In addition to in- and outpatient medical services, Shalom Clinic provides home-based supportive care for patients with acute illness, and with such provisions, it is conceivable that the instrumental and emotional support offered were associated with lowered psychological distress symptoms. Recent studies have highlighted the link between community-based supportive services and improved mental health outcomes (Rich et al., 2012; Thomson et al., 2014). The extent to which engagement in supportive services mediates the relationship between onset of illness symptoms and mental health outcomes warrants further examination.
Limitations
Several limitations of this study were noteworthy. First, findings from this cross-sectional study are based on participants sampled from families actively receiving and engaged with medical care at a community-based HIV clinic. As such, the findings could not be generalized to PLHIV in Delhi who might not be linked with medical services due to illness condition, or logistic barriers to accessing and engaging in care. Second, these findings represent a static snapshot of the relationship between food insecurity and mental health and therefore do not allow us to determine the temporal order of the associations. Third, given that the K6 and HFIAS, respectively, measure recent non-specific psychological distress and food insecurity reported in the past 30 days, our findings do not consider the potential impact of chronic poverty-related determinants of specific mental disorders. In addition, more precise measure of immunologic function such as CD4+ counts were not available, which limited conclusions drawn between the association between psychological distress and HIV illness progression. These limitations collectively highlight the importance of longitudinal study designs with a larger general sample that reflect the dynamic potential long-term risks of food insecurity (Barrett, 2010). Repeated measures studies with comparison groups are needed to evaluate mental health services that are integrated with the direct and indirect outcomes of livelihood interventions such as vocational training skills training, microfinance, food assistance, and nutritional supplementation (Anema et al., 2009; Kennedy, Fonner, O'Reilly, & Sweat, 2014). Moreover, process evaluations are needed to identify and strategically address programmatic barriers to decentralizing resources to integrate mental health interventions with socio-economic livelihood interventions (Saraceno et al., 2007). Finally, this study supports the importance of identifying factors that moderate the relationship between food insecurity and poor mental health outcomes to guide integrated mental health and livelihood interventions that specifically target a subpopulation(s) of PLHIV who are consistently hard to reach despite well-meaning community-based participatory approaches (Barrett, 2010).
Notwithstanding these limitations, the present study builds upon increasing evidence that many PLHIV in high poverty regions such as Delhi India contend with daily livelihood stressors such as food insecurity that often heightens psychological distress. Similar mounting evidence of the link between food insecurity and mental health call for concerted efforts to design, evaluate, and refine integrated HIV mental health and livelihood programming.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- 1. Aberman, N. L., Rawat, R., Drimie, S., Claros, J. M., & Kadiyala, S. (2014). Food security and nutrition interventions in response to the AIDS epidemic: Assessming global action and evidence. AIDS & Behavior, 18, S554–S565. doi: 10.1007/s10461-014-0822-z [CrossRef], [PubMed], [Web of Science ®]
- 2. Anderson, S. A. (1990). Core indicators of nutritional state for difficult-to-sample populations. Journal of Nutrition, 120(11), 1555–1160.
- 3. Anema, A., Vogenthaler, N., Frongillo, E. A., Kadiyala, S., & Weiser, S. D. (2009). Food insecurity and HIV/AIDS: Current knowledge, gaps, and research priorities. Current HIV/AIDS Reports, 6, 224–231. doi: 10.1007/s11904-009-0030-z [CrossRef], [PubMed]
- 4. Baro, M., & Deubel, T. F. (2006). Persistent hunger: Perspectives on vulnerability, famine, and food security in sub-Saharan Africa. Annual Review of Anthropology, 35, 521–538. doi: 10.1146/annurev.anthro.35.081705.123224 [CrossRef], [Web of Science ®]
- 5. Barrett, C. B. (2010). Measuring food insecurity. Science, 327, 825–828. doi: 10.1126/science.1182768 [CrossRef], [PubMed], [Web of Science ®]
- 6. Browne, M. W., & Cudeck, R. (1990). Single sample cross-validation indices for covariance structures. Multivariate Behavioral Research, 24, 445–455. doi: 10.1207/s15327906mbr2404_4 [Taylor & Francis Online], [Web of Science ®]
- 7. Bukusuba, J., Kikafunda, J. K., & Whitehead, R. G. (2007). Food security status in households of people living with HIV/AIDS (PLWHA) in a Ugandan urban setting. British Journal of Nutrition, 98, 211–217. doi: 10.1017/S0007114507691806 [CrossRef], [PubMed], [Web of Science ®]
- 8. Chandra, P. S., Ravi, V., Desai, A., & Subbakrishna, D. K. (1998). Anxiety and depression among HIV-infected heterosexuals – A report from India. Journal of Psychosomatic Research, 45(5), 401–409. doi: 10.1016/S0022-3999(98)00028-2 [CrossRef], [PubMed], [Web of Science ®], [CSA]
- 9. Coates, J., Swindale, A., & Blinsky, P. (2007). Household Food Insecurity Access Scale (HFIAS) for measurement of household food access: Indicator guide (v. 3). Washington, DC: Food and Nutrition Technical Assistance Project, Academy for Education Development.
- 10. Das, J., Do, Q. T., Friedman, J., McKenzie, D., & Scott, K. (2007). Mental health and poverty in developing countries: Revisiting the relationship. Social Science and Medicine, 65(2007), 467–480. doi: 10.1016/j.socscimed.2007.02.037 [CrossRef], [PubMed], [Web of Science ®]
- 11. Filmer, D., & Pritchett, L. H. (2001). Estimating wealth effects without expenditure data or tears: An application of educational enrollments in states of India. Demography, 38(1), 115–132. [PubMed], [Web of Science ®], [CSA]
- 12. Hadley, C., & Patil, C. L. (2006). Food insecurity in rural Tanzania is associated with maternal anxiety and depression. American Journal of Human Biology, 18, 359–368. doi: 10.1002/ajhb.20505 [CrossRef], [PubMed], [Web of Science ®]
- 13. Hadley, C., Tegegn, A., Tessema, F., Cowan, J. A., Asefa, M., & Galea, S. (2008). Food insecurity, stressful life events and symptoms of anxiety and depression in east Africa: Evidence from the Gilgel Gibe growth and development study. Journal of Epidemiology and Community Health, 62, 980–986. doi: 10.1136/jech.2007.068460 [CrossRef], [PubMed], [Web of Science ®]
- 14. Heylen, E., Panicker, S. T., Chandy, S., Steward, W. T., & Ekstrand, M. L. (2014). Food insecurity and its relation to psychological well-being among South Indian people living with HIV. AIDS & Behavior, 19, 1548–1558. doi:10.1007/s10461-014-0966-x [CrossRef], [Web of Science ®]
- 15. Jagannath, V., Unniskrishnan, B., Hegde, S., Ramapuram, J. T., Roa, S., Achappa, B., … Kotian, M. S. (2011). Association of depression with social support and self-esteem among HIV positives. Asian Journal of Psychiatry, 4, 288–292. doi: 10.1016/j.ajp.2011.10.006 [CrossRef], [PubMed]
- 16. Kamath, R., Robin, S., & Chandrasekaran, V. (2014). Common mental disorders: A challenge among people living with HIV/AIDS in Udupi, India. Annals of Medical and Health Sciences Research, 4(2), 242–247. doi: 10.4103/2141-9248.129051 [CrossRef]
- 17. Kennedy, C. E., Fonner, V. A., O'Reilly, K. R., & Sweat, M. D. (2014). A systematic review of income generation interventions, including microfinance and vocational skills training, for HIV prevention. AIDS Care, 26(6), 659–673. doi: 10.1080/09540121.2013.845287 [Taylor & Francis Online], [PubMed], [Web of Science ®]
- 18. Kessler, R. C., Barker, P. R., Colpe, L. J., Epstein, J. F., Gfroerer, J. C., Hiripi, E., … Zaslavsky, A. M. (2003). Screening for serious mental illness in the general population. Archives of General Psychiatry, 62, 593–602. doi: 10.1001/archpsyc.62.6.593 [CrossRef], [Web of Science ®]
- 19. Kessler, R. C., Green, G. J., Gruber, M. J., Sampson, N. A., Bromet, E., Cuitan, M., … Zaslavsky, A. M. (2010). Screening for serious mental illness in the general population with the K6 screening scale: Results from the WHO World Mental Health (WMH) survey initiative. International Journal of Methods in Psychiatric Research, 19(Suppl 1), 4–22. doi: 10.1002/mpr.310 [CrossRef], [PubMed], [Web of Science ®]
- 20. Lund, C., Breen, A., Flisher, A. J., Kakuma, R., Corrigall, J., Joska, J. A., … Patel, V. (2010). Poverty and common mental disorders in low and middle income countries: A systematic review. Social Science and Medicine, 71(2010), 517–528. doi: 10.1016/j.socscimed.2010.04.027 [CrossRef], [PubMed], [Web of Science ®]
- 21. Maxwell, S., & Smith, M. (1992). Household food security: A conceptual review. In S. Maxwell & T. Frankenberger (Eds.), Household Food Security: Concepts, Indicators, Measurements: A Technical Review (pp. 19–33). Rome and New York: IFAD and UNICEF.
- 22. Mayston, R., Patel, V., Abas, M., Korgaonkar, P., Paranjape, R., Rodrigues, S., & Prince, M. (2014). Psychological predictors for attendance of post-HIV test counselling and linkage to care: The Umeed cohort study in Goa, India. BMC Psychiatry, 14, 188–198. doi: 10.1186/1471-244X-14-188 [CrossRef], [PubMed], [Web of Science ®]
- 23. Muthén, L. K., & Muthén, B. O. (2012). Mplus user’s guide (7th ed.). Los Angeles: Muthén & Muthén.
- 24. Myer, L., Stein, D. J., Grimsrud, A., Seedat, S., & Williams, D. R. (2008). Social determinants of psychological distress in a nationally representative sample of South African adults. Social Science and Medicine, 66(8), 1828–1840. doi: 10.1016/j.socscimed.2008.01.025 [CrossRef], [PubMed], [Web of Science ®]
- 25. Nanama, S., & Frongillo, E. A. (2012). Altered social cohesion and adverse psychological experiences with chronic food insecurity in the non-market economy and complex households in Burkina Faso. Social Science and Medicine, 74, 444–451. doi: 10.1016/j.socscimed.2011.11.009 [CrossRef], [PubMed], [Web of Science ®]
- 26. Patel, V. (2007). Mental health in low- and middle-income countries. British Medical Bulletin, 81–82, 81–96. doi: 10.1093/bmb/ldm010 [CrossRef], [PubMed], [Web of Science ®]
- 27. Patel, V., Kirkwood, B. R., Pednekar, S., Weiss, H., & Mabey, D. (2006). Risk factors for common mental disorders in women: Population-based longitudinal study. The British Journal of Psychiatry, 189, 547–555. doi: 10.1192/bjp.bp.106.022558 [CrossRef], [PubMed], [Web of Science ®]
- 28. Patel, V., & Kleinman, A. (2003). Poverty and common mental disorders in developing countries. Bulletin of the World Health Organization, 81, 609–615. [PubMed], [Web of Science ®]
- 29. Rich, M. L., Miller, A. C., Niyigena, P., Franke, M. F., Niyonzima, J. B., & Socci, A. R. (2012). Excellent clinical outcomes and high retention in care among adults in a community-based HIV treatment program in rural Rwanda. JAIDS, 59(3), e35–42.
- 30. Sahn, D. E., & Stifel, D. (2003). Exploring alternative measures of welfare in the absence of expenditure data. Review of Income and Wealth, 49(4), 463–489. doi: 10.1111/j.0034-6586.2003.00100.x [CrossRef]
- 31. Saraceno, B., van Ommeren, M., Batniji, R., Cohen, A., Gureje, O., Mahoney, J., … Underhill, C. (2007). Barriers to improvement of mental health services in low-income countries. Lancet, 370, 1164–1174. doi: 10.1016/S0140-6736(07)61263-X [CrossRef], [PubMed], [Web of Science ®]
- 32. Subbaraman, R., Nolan, L., Shitole, T., Sawant, K., Shitole, S., Sood, K., … Patil-Deshmukh, A. (2014). The psychological toll of slum living in Mumbai, India: A mixed methods study. Social Science and Medicine, 119(2014), 155–169. doi: 10.1016/j.socscimed.2014.08.021 [CrossRef], [PubMed], [Web of Science ®]
- 33. Thomson, D. R., Rich, M. L., Kaigamba, F., Socci, A. R., Hakizamunga, M., Bagiruwigize, E., … Franke, M. F. (2014). Community-based accompaniment and psychosocial health outcomes in HIV-infected adults in Rwanda: A prospective study. AIDS Behavior, 18, 368–380. doi: 10.1007/s10461-013-0431-2 [CrossRef], [PubMed], [Web of Science ®]
- 34. Tsai, A. C., Bangsberg, D. R., Frongillo, E. A., Hunt, P. W., Muzoora, C., Martin, J. N., & Weiser, S. D. (2012). Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Social Science and Medicine, 74(12), 2012–2019. doi: 10.1016/j.socscimed.2012.02.033 [CrossRef], [PubMed], [Web of Science ®]
- 35. UNAIDS. (2014). Gap report. Geneva, Switzerland: UNAIDS. Retrieved from http://www.unaids.org/sites/default/files/media_asset/UNAIDS_Gap_report_en.pdf.
- 36. United Nations. (2014). The millennium development goals report. New York: United Nations.
37. United Nations Development Programme. (2012). A review of socio-economic empowerment initiatives for women living with HIV in Asia. Bangkok, Thailand: UNDP. - 38. Weaver, L. J., & Hadley, C. (2009). Moving beyond hunger and nutrition: A systematic review of the evidence linking food insecurity and mental health in developing countries. Ecology of Food and Nutrition, 48(4), 263–284. doi: 10.1080/03670240903001167 [Taylor & Francis Online], [PubMed], [Web of Science ®]
- 39. World Health Organization. (2003). Organization of services for mental health. (Mental Health Policy and Service Guidance Project, Trans.). Geneva: Author.
- 40. Zelaya, C. E., Sivaram, S., Johnson, S. C., Srikrishnan, A. K., Suniti, S., & Celentano, D. D. (2012). Measurement of self, experienced, and perceived HIV/AIDS stigma using parallel scales in Chennai, India. AIDS Care, 24(7), 846–855. doi: 10.1080/09540121.2011.647674 [Taylor & Francis Online], [PubMed], [Web of Science ®]